Summary of standards to be assessed 2026
The Approved Provider Scheme is based on a set of standards that encompass the six domains, these have been detailed below.
Headway is managing this project with the experience of the Service User and their family / carer as its main priority. The standards selected for evaluation within each of the below domains reflect the need for primary and fundamental care / choice and dignity issues being central to the care provided.
DOMAIN 1 – CULTURE
AP 1 – Service Philosophy & Ethos
A clear philosophy guides the service. Staff understand it, believe in it, and bring it to life through their daily actions.
Key elements:
- A shared ethos rooted in dignity, empowerment, and inclusion
- Philosophy evident in practice, not just policy
- Accessible information for service users and families
- Openness, honesty, and transparency in every interaction
- Values introduced at induction and reinforced over time
AP 2 – Dignity, Privacy and Care
People feel respected, safe, and in control. Support is delivered with sensitivity and in a way that protects privacy and promotes independence.
Key elements:
- Care plans shaped around personal preferences and ABI needs
- Service users actively involved in decisions
- Consistent safeguarding of dignity during all tasks
- Awareness of cultural and identity-based needs
- Staff understand the emotional impact of ABI and respond supportively
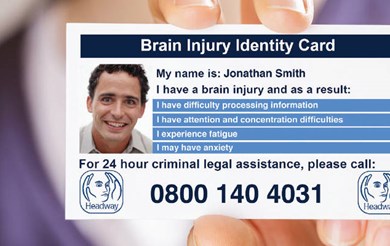
AP 3 – ABI Awareness for Service Users & Families
Staff help individuals and families understand brain injury in a meaningful, accessible way.
Key elements:
- Clear explanations of cognitive, emotional, and behavioural changes
- Supportive conversations using plain and respectful language
- Written or visual resources for families
- Staff apply ABI knowledge to real-life situations
- Services promote understanding, not blame
AP 4 – Service Initiatives
The service actively looks for ways to grow, innovate, and enhance wellbeing.
Key elements:
- Cognitive rehabilitation initiatives or structured supports
- Family involvement strengthened through workshops or meetings
- Staff learning beyond mandatory training (webinars, conferences)
- Wellbeing initiatives for the staff team
- Links with external organisations, including vocational or community partners
DOMAIN 2 – SYSTEMS & PROCESSES
This Domain looks at how well the service is organised, led, and supported. Strong, reliable systems ensure safe and effective care.
AP 5 – Management
Leaders model positive practice and create a stable, supportive environment for staff and service users.
Key elements:
- Managers understand ABI and support staff with confidence
- Clear approaches to quality monitoring and improvement
- Strong safeguarding processes
- Open, respectful communication
- A focus on supporting staff learning, resilience, and wellbeing
AP 6 – Staff Selection, Recruitment & Ratio
The service recruits people with the right values and maintains staffing levels that support emotional, cognitive, and social needs—not just physical care.
Key elements:
- Recruitment emphasises empathy, patience, flexibility, and communication
- Service users involved in recruitment or probation where possible
- Induction and shadowing tailored to ABI learning needs
- Safe and meaningful staff-to-service user ratios
- Teams selected to support consistency and relationship-building
AP 7 – Key Worker Allocation
Every service user has a designated key worker who supports coordination, communication, and personalised care.
Key elements:
- Allocation based on skills, compatibility, and communication style
- Key workers maintain regular contact with families
- Key workers contribute to reviews and goal setting
- Clear expectations and support for key worker role
AP 8 – Pre-admission Assessment
Before someone moves in, the service ensures it understands their needs—and that it can meet them safely and well.
Key elements:
- Assessment considers cognitive, emotional, behavioural, physical, and sensory needs
- Information gathered from professionals, families, and records
- Environment prepared in advance of admission
- Staff briefed and trained on individual needs
- Smooth and supportive transition into the service
AP 9 – Care Plan
Care plans are person-centred, practical, and shaped by the unique impact of the individual’s brain injury.
Key elements:
- Clear, step-by-step strategies to support daily living
- Links between goals, risks, and support strategies
- Emotional and behavioural needs clearly described
- Evidence of shared decision-making
- Adjusted for fatigue, cognitive load, and therapeutic advice
AP 10 – Mental Capacity Act / DoLS or Equivalent
Capacity assessments and best-interest decisions take into account the hidden effects of brain injury and use appropriate adaptations.
Key elements:
- Staff understand the frontal lobe paradox and cognitive fatigue
- Adaptations (visual aids, simplified language, pacing, repetition)
- Interpreters or bilingual support used where needed
- Clear documentation of decisions and involvement
- Regular review of DoLS or equivalents
AP 11 – Discharge / Home Overnight Stays
Transitions are planned and supported to ensure safety, consistency, and confidence.
Key elements:
- Gradual transition planning
- Family training on equipment, routines, and strategies
- Coordinated communication with next providers
- Signposting to community and statutory services
- Respectful conversations about readiness and expectations
AP 12 – Daily Records
Daily notes are clear, objective, and helpful. They reflect ABI-specific needs, progress, and challenges.
Key elements:
- Notes include levels of prompting, cues, and engagement
- Observations recorded without judgement
- Evidence of strategy use (memory aids, pacing, communication tools)
- Recording of changes, triggers, improvements or concerns
- Notes support reflection and consistent team practice
AP 13 – Service Provider Reflection & Feedback
The service actively listens, reflects, and improves.
Key elements:
- Opportunities for service users to give feedback (including easy-read options)
- Family input offered through flexible formats
- Staff reflections valued and acted upon
- Evidence of real changes resulting from feedback
- A culture of openness and shared learning
DOMAIN 3 – WORKFORCE DEVELOPMENT
This Domain focuses on how well staff are trained, supported, and developed.
People affected by brain injury deserve consistent, confident, and informed care.
A skilled and supported workforce is at the heart of delivering this.
AP 14 – Staff Induction, Evaluation & Feedback
A strong induction helps staff feel welcomed, supported, and confident. It ensures they understand the unique needs associated with acquired brain injury and feel equipped to provide safe and meaningful support.
Key elements:
- A structured induction that introduces ABI principles in a clear and accessible way
- Shadowing opportunities with experienced ABI staff
- Early competency checks and reflective conversations
- Space for new starters to ask questions, share concerns, and reflect
- Induction adapted to individual learning needs and styles
- Warm, supportive onboarding that prioritises confidence as well as knowledge
AP 15 – Post-Induction ABI Training & Ongoing Development
Staff continue to grow in confidence and skill after induction. Training is relevant, practical, and clearly linked to the daily needs of the people they support.
Key elements:
- At least 80% compliance with ABI post-induction training modules
- Modules cover core cognitive domains (memory, attention, fatigue, executive functions, communication, behaviour, emotional regulation, visual processing, quality of life, sex and sexuality)
- Regular refresher training to strengthen practice and avoid complacency
- Evidence that staff apply learning in real situations — not just complete courses
- Opportunities for additional development such as webinars, conferences, and external qualifications
- Supportive supervision that encourages reflection, confidence, and growth
- A strong culture of learning that values curiosity, compassion, and good practice
DOMAIN 4 – SERVICE DELIVERY
This Domain explores how the service understands and meets the day-to-day rehabilitation, emotional, behavioural, and therapeutic needs of people with an acquired brain injury.
It focuses on meaningful, person-centred support that reflects the complexity of ABI.
AP 16 – Cognitive Needs
Staff understand how brain injury affects memory, attention, executive functioning, communication, fatigue, and visual processing. They use this knowledge to support people with confidence and compassion.
Key elements:
- Staff can clearly describe the individual’s cognitive profile
- Day-to-day support reflects the person’s strengths and needs
- Strategies used consistently (e.g., prompts, pacing, visual cues, repetition)
- Staff adapt communication based on processing speed and comprehension
- Cognitive rehabilitation supported where appropriate (tasks, groups, technology)
- Fatigue monitored and managed with flexibility and sensitivity
- Evidence of collaboration with therapists where available
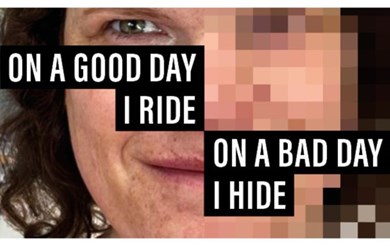
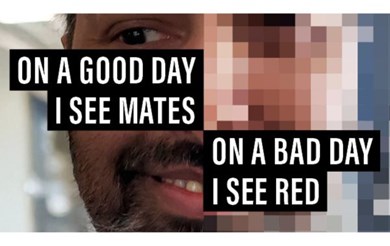
AP 17 – Emotional Support
People receive the emotional support they need to manage the psychological impact of ABI. Care is grounded in empathy, respect, and awareness of how emotions influence behaviour and engagement.
Key elements:
- Staff trained to recognise emotional changes following ABI
- Support aligns with guidance from psychology or mental health professionals
- Emotionally supportive approaches used in daily interactions
- People encouraged to express feelings safely and at their own pace
- Staff understand links between fatigue, frustration, anxiety, and overwhelm
- Opportunities for meaningful connection, reassurance, and validation
AP 18 – Behaviours That Challenge
Support for behaviour is proactive, compassionate, and grounded in an understanding of brain injury. Staff see behaviour as communication, not “non-compliance.”
Key elements:
- Behaviour support plans tailored to ABI-related triggers and needs
- Staff trained in both proactive and reactive strategies
- Clear, concise risk assessments informed by therapy or clinical guidance
- Data, trends, and outcomes monitored and reviewed
- Incidents explored in a learning-focused, supportive way
- Staff encouraged to remain calm, consistent, and non-judgemental
- Positive Behaviour Support principles reflected in daily practice
AP 19 – Reablement & Therapy Input
Reablement and therapy support help people regain confidence, skills, and independence. Access to therapy—whether in-house or externally arranged—is clear and well communicated.
Key elements:
- Clear pathways for accessing therapy (in-house, external, or commissioned)
- Staff understand therapy goals and integrate strategies into daily routines
- Reablement tasks are meaningful, achievable, and person-centred
- Communication between therapy and support staff is timely and effective
- Consistent use of equipment, technology, or aids
- Evidence of progress, no matter how small, celebrated and recorded
- Flexibility in approach based on fatigue and emotional readiness
DOMAIN 5 – PROMOTING QUALITY OF LIFE
This Domain focuses on what makes life meaningful, enjoyable, and fulfilling for people with brain injuries. It highlights choice, independence, relationships, identity, activity, and wellbeing.
Quality of life is central to rehabilitation, recovery, and long-term happiness.
AP 20 – Goal Setting & Outcome Monitoring
People are supported to set goals that matter to them. Progress is monitored in a way that is clear, consistent, and meaningful.
Key elements:
- Goals reflect personal interests, strengths, and values
- Use of structured goal-setting tools specific to ABI
- Short- and long-term goals reviewed with the person and key staff
- Monitoring considers fatigue, motivation, and cognitive load
- Evidence that all staff understand and support active goals
- Achievements celebrated — including small steps forward
AP 21 – Personal Choices & Meaningful Activities
People have real choice and control over how they spend their time. Activities are meaningful, enjoyable, and aligned with personal interests and cultural identity.
Key elements:
- Activities chosen with the person, not for the person
- Options include social, cognitive, creative, sensory, and community-based activities
- Support staff understand the impact of fatigue and pace activities accordingly
- Independence encouraged wherever possible
- Positive risk-taking supported in a safe, thoughtful way
- Weekly routines feel purposeful, balanced, and varied
AP 22 – Safe Internet Use & Digital Access
People are supported to access the digital world safely, confidently, and with the right level of supervision. The service recognises the role of technology in communication, learning, leisure, and independence.
Key elements:
- Clear guidance on safe internet use
- Digital access adapted to cognitive and communication needs
- Safeguards in place (parental controls, protected Wi-Fi, safe browsing tools)
- Support to use devices safely, including tablets or computers provided by the service if needed
- Understanding of online risks, especially related to vulnerability, consent, and exploitation
- Person-centred approach that promotes autonomy while reducing harm
AP 23 – Promotion of an Active Lifestyle
Movement and physical activity are encouraged in ways that are safe, enjoyable, and accessible to all.
Key elements:
- Activities tailored to individual ability, including wheelchair-friendly options
- Support for mobility, balance, coordination, and endurance
- Staff recognise fatigue patterns and adjust expectations
- Opportunities for both structured exercise and everyday movement
- Encouragement to stay active in the service and the community
AP 24 – Vocational, Volunteering & Educational Opportunities
People who want to engage in work, volunteering, or education are supported to explore their aspirations confidently and safely.
Key elements:
- Assessment of interests, skills, and support needs
- Links with employers, community groups, and education providers
- Help to develop confidence, communication, and independence
- Reasonable adjustments discussed and supported
- Collaboration with external professionals where needed
- Support for meaningful roles, no matter the level of ability
AP 25 – Menu Choices & Mealtime Support
Meals are nutritious, enjoyable, and culturally respectful. Mealtimes support health, dignity, and rehabilitation.
Key elements:
- Varied and culturally appropriate menu choices
- Attractive, appetising food presentation
- Sensitivity to individual needs and preferences
- Support for people with swallowing or nutritional needs
- Staff know when to seek advice from SALT, dietetics, or medical professionals
- Mealtimes are viewed as both social and therapeutic opportunities
AP 26 – Spiritual, Cultural & Social Identity
Each person’s identity is respected and supported. The service helps people maintain or reconnect with their beliefs, traditions, and communities.
Key elements:
- Support for cultural practices, food preferences, clothing, and traditions
- Opportunities to access spiritual or religious expression
- Invitations extended to local faith or cultural representatives (with consent)
- Respect for diversity, individuality, and personal history
- Environments that feel inclusive and meaningful
AP 27 – Sexual Identity & Needs
People receive sensitive, respectful support around sexuality, identity, and relationships. Staff work safely, professionally, and without judgement.
Key elements:
- Staff understand the difference between sexual expression and risky behaviour
- Support with online safety, dating apps, building relationships, and appropriate boundaries
- Guidance sought from senior staff or clinicians where needed
- Cultural, personal, or religious values of staff do not influence support offered
- Clear, person-centred approaches aligned with care plans
- Open, safe conversations around consent, privacy, and dignity
DOMAIN 6 – ENVIRONMENT & COMMUNITY INTEGRATION
This Domain focuses on the spaces people live in and the way services help individuals feel connected, confident, and included in their local community. A well-designed environment and a sense of belonging can have a powerful impact on rehabilitation, identity, and wellbeing.
AP 28 – Buildings & External Spaces
The environment is safe, welcoming, and designed to support people with brain injuries. It feels homely, comfortable, and inclusive, while meeting all relevant safety and accessibility standards.
Key elements:
- Communal areas are clean, warm, and comfortable for visitors
- Bedrooms, studios, or flats can accommodate overnight stays for partners or relatives where appropriate
- Outdoor areas are well maintained, safe, and accessible
- The layout supports independence and orientation
- Maintenance is proactive and responsive
- People have input into personalising their own space
AP 29 – Supporting Environment
The environment actively helps people navigate their day, remember routines, and feel confident. Spaces are designed with ABI needs in mind, especially around memory, attention, communication, and sensory impact.
Key elements:
- Clear signage for exits, toilets, communal spaces, and private rooms
- Whiteboards or visual aids showing daily routines, staff on duty, meals, and activities
- Photos of past events with names, dates, and locations to support memory recall
- Access to adaptive technology (e.g., tablets, apps, Alexa, timers, digital reminders)
- Staff trained to use assistive equipment confidently and safely
- Equipment stored appropriately and maintained to a high standard
AP 30 – Community Integration
People feel part of their local community. They are supported to access meaningful places, activities, and opportunities outside the service. Community involvement strengthens identity, independence, confidence, and wellbeing.
Key elements:
- Regular access to community spaces such as cafés, gyms, parks, libraries, shops, and social groups
- Support for safe use of public transport or accessible alternatives
- The service has access to its own adapted or accessible vehicle where possible to broaden opportunities
- Activities planned around the person’s interests, abilities, and culture
- Positive risk-taking supported thoughtfully and safely
- Staff help build confidence, reduce anxiety, and celebrate achievements
- Relationships with local organisations, charities, or community groups
- Support tailored to fluctuating fatigue, emotional needs, and cognitive load