Luke added:
“Rehabilitation is a long-term commitment, and this guidance specifies the joined-up approach we’ve been demanding for many years.
“Some of the recommendations contained within the guidelines could be truly transformative. However, the potential gains to brain injury survivors, their families and carers, and indeed the public purse will only be realised if the guidelines are acted upon by the government and commissioning bodies.
“In essence, they have to be backed by meaningful investment in community-based rehabilitation.”
The new guidance on rehabilitation for those living with acquired brain injury was published on 15 October 2025. This guidance sets out a vision for person-centred, coordinated and lifelong rehabilitation across hospital, community and social care settings.
Among its most eye-catching recommendations is the appointment of a complex case manager with specialist knowledge in both inpatient and community-based rehabilitation. These single points of contact are intended to provide advice, proactive support and signposting – effectively coordinating rehabilitation across multiple services.
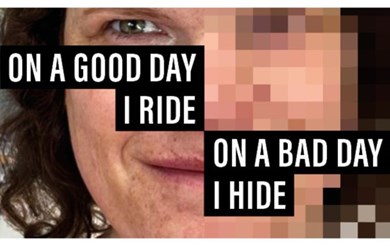
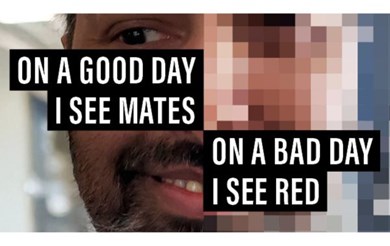
The guideline also highlights the importance of holistic assessments, rehabilitation passports, and interventions that address not only physical recovery but also emotional, cognitive, communication and social needs. This includes access to speech and language therapy.
Taken together, these proposals offer a practical and compassionate framework for lifelong rehabilitation. However, the obvious and fundamental questions remain: where will these case managers come from in an already stretched social care landscape? And how will this additional resource be funded?
With someone admitted to a UK hospital every 90 seconds with a brain injury – nearly 1,000 people every day – and many requiring ongoing rehabilitation after discharge, the scale of need is immense. Yet, at a time when local community-based rehabilitation services are closing due to unsustainable funding, the gap between ambition and reality is widening.
Local Headway charities are a lifeline for brain injury survivors and help ease pressure on overstretched statutory services. They deliver vital rehabilitation and community support, but many are struggling to survive. Chronic underfunding leaves them carrying unsustainable costs, even though they prevent more costly reliance on health and social care systems.
“In contrast to the ambitious aims of the new NICE guideline, we are witnessing a crisis in community-based services unfolding in real time.
“Specialist services for brain injury survivors are being forced to close due to rising costs and chronic underfunding. Instead of advancing towards better care, we are regressing.
“The gap between the guideline’s aspirations and the reality on the ground is widening by the day.
“We warmly welcome the new guideline from NICE, which sets a vital benchmark for rehabilitative care – one that could reshape services for the better.
“But without urgent action and sustained investment, these standards will remain aspirational rather than achievable.
“Its publication is timely, coming as it does before the Government publishes its long-awaited Acquired Brain Injury Action Plan.
“We will be encouraging Ministers to considering carefully the recommendations of NICE and urging them to take the bold action that is so desperately needed to curb the serious threat to the future of community-based support.
“If they fail to act now, the community-based services that underpin lifelong rehabilitation will continue to diminish before our eyes, taking with them the very foundations needed to realise the promise of the guideline.”
Back