Abstract
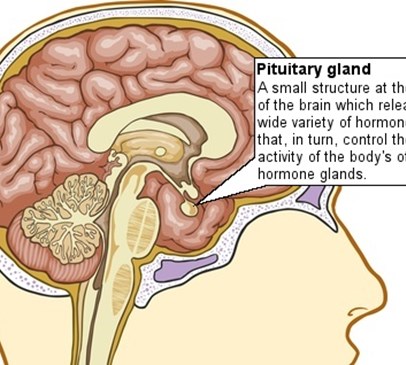
PURPOSE: Hypopituitarism has been reported in up to half of long-term survivors of traumatic brain injury. We attempted to define the natural history of post-traumatic hypopituitarism to devise guidelines for the optimal timing of patients' assessment and hormone replacement.
SUBJECTS AND METHODS: Fifty consecutive patients with severe or moderate head trauma were enrolled in a prospective study of pituitary function during the acute phase, at 6 months, and at 12 months after injury. Growth hormone and adrenocorticotropin hormone reserves were assessed using the glucagon stimulation test. Baseline serum concentrations of other anterior pituitary hormones were measured. Results were compared with normative data obtained from matched healthy controls.
RESULTS: Nine patients (18%) had growth hormone deficiency in the acute phase; at 6 months, 5 patients recovered function and 2 new deficiencies were detected; at 12 months, 1 patient recovered, leaving 5 patients (10%) with growth hormone deficiency. Eight patients (16%) showed subnormal cortisol response in the acute phase; at 6 months, 4 patients had recovered and 5 new deficiencies were detected; all 9 patients had persistent abnormalities at 2 months. Forty patients (80%) had gonadotropin deficiency in the acute phase, of whom 29 (73%) recovered by 6 months and 34 (85%) recovered by 12 months. Thyrotropin deficiency was present in 1 patient in the acute phase, who recovered by 6 months; 1 new case was diagnosed at 6 months, which persisted at 12 months.
CONCLUSION: After traumatic brain injury, early neuroendocrine abnormalities are sometimes transient, whereas late abnormalities present during the course of rehabilitation. A follow-up strategy with periodic evaluation is a necessary part of the optimal care for patients with traumatic brain injury.
Reference
Agha, A., Phillips, J., O'Kelly, P., Tormey, W. and Thompson, CJ (2005) The natural history of post-traumatic hypopituitarism: implications for assessment and treatment.Am J Med 118 (12):1416.
Back