Coma and prolonged disorders or consciousness (PDOC)
In cases of serious injury to the brain, there may be a significant period of loss of consciousness or altered state of consciousness. These are known as comas and prolonged disorders of consciousness (PDOCs).
Having a loved one in a coma or state of PDOC can be extremely distressing. It might be difficult to know how best to support your loved one, as well as how to cope with your own change in circumstances and emotions. One of the most upsetting things about having a loved one in a coma or state of PDOC is not knowing if and when they will regain consciousness, and how they may be afterwards.
Headway has a number of services that can help out at this difficult time, which you can find more information on in the sections below.
Read on to find out about these states and how you can support both yourself and your loved one at this difficult time.
In this section:
Coma after brain injury
The information provided below explains what a coma is and how you can support your loved one and yourself through this difficult time. For more detailed information about comas, including treatment, outcomes and next steps, see our publication Coma after brain injury.
What is a coma?
In cases of serious injury to the brain, for example following a road traffic collision, a stroke or an anoxic brain injury, an immediate consequence can be a loss of consciousness. If this lasts for longer than 6 hours, the person is in a coma.
When in a coma, a person may look like they are asleep, but they cannot be woken up. They do not respond to any stimuli, such as touch, light or sound, nor can they make any intentional or purposeful movements. They may cough or swallow, but these are reflexive and not intentional.
Unfortunately, nobody can tell how long a coma will last for. In many cases they last for a few weeks, but this can be much shorter or longer, and will depend upon factors such as the person’s age and the extent of their brain injury.
What is an induced coma?
An induced coma is different to the type of coma that someone naturally falls into after brain injury. A person in an induced coma will have intentionally been placed into this state by clinicians at the hospital. This will be done by administering specialist medications. It will be temporary and carefully controlled.
A person will be placed into an induced coma if it will help to prevent further damage from being sustained to the brain, and to help with recovering after serious illness or injury.
The person’s condition will be closely monitored throughout this process, and when they are ‘woken up’, this will be done very gradually by slowly reducing the medications.
A person being woken up from an induced coma may initially appear confused and distressed, and they might need to be sedated. This can be very concerning for families but be assured that it is a normal procedure. Your loved one will not be kept in the induced coma for any longer than is necessary.
Being involved in your loved one’s care during a coma
It is natural for people to want to be involved in their loved one’s care, as this can help them to feel more connected and helpful.
You could ask nursing staff if there are ways for you to help with basic nursing tasks, such as wiping your loved one’s face or brushing their hair. You should also be involved in discussions about their treatment, as families can often offer helpful information regarding the patient’s wishes and preferences.
Some people feel that presenting their loved one with familiar stimuli might help them to emerge from the coma - for example, playing music that they enjoy, reading to them from their favourite books, talking to them about daily events, showing them personal photographs or placing familiar objects in their hands. These activities form the basis of what is called a coma stimulation programme.
Coma stimulation programmes offer a chance to get involved in your loved one’s care, but there is limited evidence for their effectiveness. However, you can still ask nursing staff about this if you think it will be a helpful way for you to get involved.
Emerging from a coma
The term for ‘waking up’ from a coma is ‘emerging’ from a coma.
Unfortunately, it is impossible to tell if and when a person will emerge from a coma. However, if they do emerge, they will not suddenly sit up or start asking questions, like we sometimes see in films.
In most cases, a person will emerge from their coma and begin to regain consciousness, although they will be very confused at first about where they are and what has happened.
In some cases, a person will not immediately begin to regain consciousness, but will instead progress into a vegetative state (VS) or a minimally conscious state (MCS). These are called prolonged disorders of consciousness (PDOC). In a state of PDOC, the person is no longer in a coma, but they are not yet fully alert or conscious. Further information about these states is available in our publication Prolonged disorders of consciousness after brain injury.
They might also behave unusually, for example they might shout, swear, try to pull hospital tubes out or behave inappropriately. This can be very upsetting for family, especially if the behaviour is out of character. Be assured however that it is a normal and temporary part of the recovery process known as post-traumatic amnesia. Your loved one is not intentionally behaving in this way and probably will not remember their behaviour during this time. More information on this stage is available in our publication Post-traumatic amnesia after brain injury.
A person will then be transferred to a neurological ward, where their treatment will continue, and they may undergo a period of rehabilitation. More information on this stage and next steps is available in our publication Rehabilitation after brain injury.
You can find out more on our Coma - frequently asked questions page.
Prolonged disorders of consciousness (PDOCs) after brain injury
The information provided below explains what prolonged disorders of consciousness (PDOCs) are and how you can support your loved one and yourself through this difficult time. For more detailed information about PDOCs, including treatment, outcomes and next steps, see our publication Prolonged disorders of consciousness after brain injury, available from our Information Library.
What are prolonged disorders of consciousness (PDOCs)?
Prolonged disorders of consciousness (PDOCs) are states of reduced consciousness that can affect people following serious brain injury. They are distinct from a coma, which is a complete loss of consciousness lasting over 6 hours. However, many people who are initially in a coma progress to a PDOC state.
The two types of PDOCs are vegetative state and minimally conscious state.
A vegetative state (VS) is a state in which a person:
- is awake but unaware - this means that they will look like they are awake as their eyes will sometimes be open, but they will be unaware of their surroundings or themselves;
- is able to reflexively react to stimuli (such as light or sound), for instance turning their eyes towards a loud sound;
- may have some spontaneous behaviour, such as moving their arms or legs, making grunting or groaning sounds, or grinding their teeth.
Unfortunately, none of these behaviours are done with conscious intent. Therefore, while it is often tempting for family to think that someone displaying these behaviours is reacting to something they have said or done, in VS this is sadly not the case.
A minimally conscious state (MCS) is a state in which a person:
- has severely altered consciousness;
- can interact with their surroundings to some degree;
- has periods of behaving in a way that shows minimal but clear awareness of their environment or themselves.
The behaviours showing awareness and interaction are not, however, done in a consistent way.
Being involved in your loved one’s care during a PDOC
It is natural for people to want to be involved in their loved one’s care, as this can allow them to feel more connected and helpful.
You could ask nursing staff if there are ways for you to help with basic nursing tasks, such as wiping your loved one’s face or brushing their hair. You should also be involved in discussions about their treatment, as families can often offer helpful information regarding the patient’s wishes and preferences.
Some people feel that presenting their loved one with familiar stimuli might help them to emerge from a prolonged disorder of consciousness (PDOC) - for example, playing music that they enjoy, reading to them from their favourite books, talking to them about daily life events, showing them personal photographs or placing familiar objects in their hands. Unfortunately, there is limited evidence for the effectiveness of these activities, but you can still ask nursing staff about this if you think it will be a helpful way for you to get involved.
These activities might be helpful if your loved one is in a state where they are able to respond to or enjoy the stimuli you present them with. However, remember not to introduce too many of these activities to your loved one, and not to do these too often, as they will need periods of rest and may become overwhelmed if overstimulated. Occupational therapists will already be making sure that the environment is appropriately set up for your loved one’s needs. You should therefore only introduce these activities under clinical guidance.
Withdrawal of treatment
Unfortunately, in some cases of severe injury, continuing to treat someone in a coma may no longer be of any benefit to them, or may only be prolonging a death that would naturally have happened at the time of the injury. In these cases, withdrawal of the person’s care may be considered.
This is a very difficult decision to make for all involved, and will be particularly distressing for families.
Any decisions regarding withdrawal of treatment will always be made in your loved one’s best interests, for instance if their brain injury is so severe that they are unlikely to ever regain any quality of life.
Any decisions about withdrawal of treatment should always be made under medical, ethical and legal frameworks, and should involve the family and specialists.
In cases where there is a disagreement between family and the clinical team, the case can be referred to the Court of Protection and examined under legal proceedings. Loved ones are allowed to make these applications to the Court of Protection if they have concerns about withdrawal of treatment decisions.
If it is agreed that the process for withdrawal of treatment will begin, nurses should explain the next steps to you very carefully and sensitively. You will be given the chance to spend time with your loved one, and should have the opportunity to ask any questions or raise any concerns that you may have.
The change that takes place over your loved one will be gradual, over a period of days and weeks. There is no standard way that treatment is withdrawn, as this will depend upon the treatment that your loved one has been receiving.
You should be offered appropriate emotional support and information throughout this process. Remember, there is no right or wrong way to feel during this time; all emotions are understandable.
The time after the loss of a loved one is often very difficult for people. There may be many mixed emotions, and you may not even know how to feel. In addition to dealing with the emotional consequences of the loss of a loved one, people may feel traumatised or distressed by their recent experiences in hospital.
Take your time with processing your feelings and consider seeking support from bereavement services or counselling. If you are struggling, consider talking to your GP about accessing psychological support. Remember that you can also contact our helpline to talk on 0808 800 2244 or helpline@headway.org.uk.
Looking after yourself
Your top priority at this stage is likely to be the welfare of your loved one, and it is natural to want to spend most of your time at their bedside. However, it is important to focus on making an effort to look after yourself through this difficult time too.
Here are some things that you can do to look after yourself during this time:
- Take regular breaks from your loved one’s bedside. You do not have to be beside them all of the time, and will be able to cope much better if you take frequent breaks. If you want to stay on site to be close by, most hospitals have quiet rooms that you can use.
- Accept as much help as you can get from family and friends, for example accepting offers for cooking meals, cleaning the house or picking children up from school. Remember that accepting help is a sign of strength, not weakness, and your loved ones will be keen to help however they can.
- Keep your employer informed of the situation. Your employer may be able to grant you time off or change your workload so that it is more manageable for you.
- There will probably be many messages of concern and requests for updates from family and friends during this time, and responding to each of these with the same information may be tiring.
- Remember to eat a healthy, balanced diet during this time, and if possible, try to take some time to do activities that you enjoy or can help you to relax. Try not to feel guilty about this, as it is important for you to look after your wellbeing through this difficult time.
- If you jointly pay bills with your loved one and are struggling to meet payments, talk things through with your bank or service provider. It may be possible to reschedule any payments and budget for your new circumstances.
- Talk to others about how you are feeling. This can be with family, close friends, or other families in the unit if they seem comfortable with talking. Do consider, however, that everyone’s situation is different, and some families may not want to talk about their circumstances. You can also contact our nurse-led helpline for information or emotional support, or use our online communities to connect with others in similar situations.
For more information on these topics, see our freely downloadable publications Coma after brain injury and Prolonged disorders of consciousness after brain injury.
Coma - frequently asked questions
We answer some of the questions frequently asked by family and friends when they have a loved one in a coma or a prolonged state of consciousness.
Find out morePost-traumatic amnesia
Post-traumatic amnesia (PTA) is the time after a period of unconsciousness when the injured person is conscious and awake, but is behaving or talking in a bizarre or uncharacteristic manner.
Find out moreHospital treatment and early recovery
Find out moreSupporting you
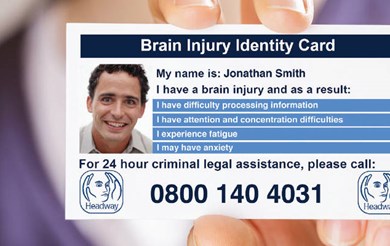
From local groups or branches, our Emergency Fund, Brain Injury Identity Card, helpline and much more, find out how Headway can support you after brain injury.
Find out more