Hypoxic and anoxic brain injury
The brain needs a continuous supply of oxygen to survive. If the oxygen supply is interrupted, the functioning of the brain is disturbed immediately and irreversible damage can quickly follow. This is known as hypoxic or anoxic brain injury.
The information on this page will be particularly useful for the family members of people who have sustained such an injury and also provides a useful starting point for professionals who wish to improve their knowledge of the subject.
All the technical terms that are used are highlighted in bold and explained on the Common brain injury terms page.
In this section:
- What is hypoxic brain injury / anoxic brain injury?
- What causes hypoxic/anoxic brain injury?
- How is hypoxic/anoxic brain injury treated?
- What are the outcomes of hypoxic/anoxic brain injury?
- Rehabilitation of hypoxic/anoxic brain injury
- What are the initial effects of hypoxic/anoxic brain injury?
- What are the long-term effects of hypoxic/anoxic brain injury?
- Get support from Headway
What is hypoxic brain injury / anoxic brain injury?
Oxygen is needed for the brain to make use of glucose, its major energy source. If the oxygen supply is interrupted, consciousness will be lost within 15 seconds and damage to the brain begins to occur after about four minutes without oxygen.
A complete interruption of the supply of oxygen to the brain is referred to as cerebral anoxia. If there is still a partial supply of oxygen, but at a level which is inadequate to maintain normal brain function, this is known as cerebral hypoxia. In practice, these two terms tend to be used interchangeably.
For the purposes of consistency, this section of the website will use the terms anoxic brain injury or cerebral anoxia, unless hypoxic injury is specifically meant.
What causes hypoxic/anoxic brain injury?
There are many potential causes of cerebral anoxia, including:
- Cardiac or respiratory arrest
- Irregular heart rhythm or poor function of the heart muscle after a heart attack, resulting in inefficient supply of blood to the brain
- Very low blood pressure (shock), resulting from blood loss (haemorrhage) or disturbed heart function
- Suffocation
- Choking
- Strangulation
- Very severe asthma attack
- Complication of general anaesthesia (where there has been inadequate oxygen supply or cardiac arrest)
- Near drowning
- Exposure to high altitudes
- Smoke inhalation
- Carbon monoxide inhalation
- Poisoning
- Drug overdose
- Electric shock
How is hypoxic/anoxic brain injury treated?
The diagnosis of an anoxic brain injury is usually quite clear at an early stage from the details of what has happened and the patient's condition on arrival at hospital. Due to the wide variety of causes of anoxia, immediate treatment will depend on the particular circumstances. In all cases, efforts will be directed at restoring a normal heartbeat, blood pressure and a good supply of oxygen to the brain.
Patients who have suffered a serious anoxic episode will usually be admitted to an intensive care unit and put on a ventilator, preferably in a specialist neurosciences centre. The patient may need drugs to maintain adequate blood pressure and normal heart beat. Seizures are quite common after an anoxic brain injury and they can be prolonged and sometimes difficult to bring under control. This is a stage of critical illness and the full range of intensive care support is needed to give the best chances of survival and the best possible outcome.
In some centres, patients may undergo medically induced cooling, referred to as therapeutic hypothermia. There is some evidence that this may have a protective effect on the brain and aid recovery by decreasing the oxygen and energy requirements of brain cells. It has been suggested that the protective effect of cooling the brain may be one reason why people sometimes survive after surprisingly long periods of immersion in very cold water. However, although therapeutic hypothermia has been known about for many years, it is still an area of controversy and can produce problems of its own, such as increased risk of infection or interference with blood clotting.
What are the outcomes of hypoxic/anoxic brain injury?
The family will want to know about the time scale of recovery after cerebral anoxia and the point at which further significant improvement becomes unlikely. As with any kind of acquired brain injury, it is difficult to give definitive rules about this.
There is some evidence that the outcome for a severe anoxic brain injury may be poorer than for a traumatic brain injury of equivalent severity, as assessed by the Glasgow Coma Scale (GCS). This may well be because of differences in the nature of the damage to the brain. In traumatic brain injury, damage to the axons (the projections that transmit messages between brain cells) is usually a prominent feature and the brain can often create alternative connections to compensate for this. In anoxic brain injury, the actual nerve cell bodies themselves are very vulnerable to damage and this damage is irreparable.
A number of factors can help to predict the outcome after cerebral anoxia:
Age
As with other forms of acquired brain injury, people over the age of 50 years tend to do less well overall than younger ones, both in terms of how likely they are to survive in the first place and in the degree of long-term recovery. However, there is evidence that older people are able to benefit from rehabilitation programmes after cerebral anoxia and so deserve equally vigorous efforts to achieve the best possible outcome.
Duration of the anoxic episode
The outcome will be determined by how extensive the damage to the brain has been. This will depend on the length of time the brain was deprived of oxygen, which can often be estimated from information about what has happened. For example, it may be known that it took 15 minutes to restore a normal heart beat after a cardiac arrest, or that someone was immersed in a swimming pool for six minutes in a near drowning incident.
Duration of coma
The duration of unconsciousness after an anoxic episode reflects the severity of the injury to the brain and helps predict the outcome. This has been studied in most detail after cardiac arrest and it has been found that only about 12% of patients who have been comatose for more than six hours after a cardiac arrest make a good recovery.
It should be noted that some comas are medically induced in order to protect the brain from further damage. The duration of a medically induced coma does not give an indication of the outcome.
Pupil reaction
Normally, the pupils will constrict when a bright light is shone into the eyes. However, following brain injury, this reflex may be lost, causing the pupils to become dilated and fixed, no longer reacting to light. This is an unfavourable sign following an anoxic brain injury and indicates a disturbance in the function of the brainstem.
Electroencephalogram (EEG)
The EEG displays the electrical activity of the brain, recorded from a set of small metal disc electrodes placed on the scalp.
There has been a good deal of research on the EEG following cardiac arrest and the degree of EEG abnormality does have some value in helping to predict the outcome. This works best at the extremes. People with a normal EEG in the early stages after cardiac arrest have a very good chance of making a full recovery and those with profoundly abnormal EEGs often either do not survive at all, or will have severe disabilities. However, there is a large group who have intermediate degrees of EEG abnormality, where the outcome is less predictable.
Brain imaging
Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) can show if there is brain swelling and give an indication of the degree of damage to the brain and the areas affected. This can help in predicting the outcome and trying to anticipate what level of neurological disability is likely in the event of survival. However, brain scans may show very little in some patients and what they show depends on the nature of the brain injury and the interval between the anoxic episode and the scan.
It is worth noting that, while there are other kinds of brain scanning techniques, such as Positron Emission Tomography (PET), functional Magnetic Resonance Imaging (fMRI), Single Photon Emission Computed Tomography (SPECT) and Magnetoencephalography (MEG), they are not usually available in hospitals and have little or no value in the assessment of brain injury. They are mainly used for research purposes.
Somatosensory evoked potentials (SSEPs)
SSEPs are the electrical responses of the brain to stimulation of the senses. They can normally be recorded from the scalp, following electrical stimulation of nerves at the wrist. These nerves transmit sensation from the arm to the brain. The absence of SSEPs recorded from the scalp is associated with a poor outcome.
Rehabilitation of hypoxic/anoxic brain injury
The principles of rehabilitation after cerebral anoxia are the same as for other types of acquired brain injury. The goal is to provide support from an integrated team with a range of specialist skills, able to help with the different problems which may occur and to support each individual to achieve the best possible outcome.
The outlook for anoxic brain injury can be uncertain and different specialists have expressed quite varied views on the timescale of recovery, based on their own individual experiences. Good improvement within the first month after an anoxic episode suggests that the outcome may be more favourable.
The most rapid recovery is usually in the first six months, and by about one year the likely long-term outcome will have become clearer. However, improvement may continue for much longer after brain injury, certainly for several years, although the steps may become more modest and gradual after the first few months. Adequate rehabilitation from the earliest possible stage is vital in order to achieve the best outcome.
What are the initial effects of hypoxic/anoxic brain injury?
The effects of hypoxic or anoxic brain injury, where the brain is starved of oxygen, can range from mild, short-term symptoms such as dizziness or concentration problems, through to severe, long-term issues including vision, speech and memory.
The body will respond to cerebral anoxia by increasing blood flow to the brain in an attempt to restore an adequate supply of oxygen. However, it is only possible to increase brain blood flow to about twice the normal level. If this is not enough to compensate for the anoxia, brain function will be disturbed and symptoms will become apparent.
Mild hypoxic/anoxic brain injury
If the cerebral anoxia is mild, there will be problems with concentration, attention, co-ordination and short-term memory, which may be relatively subtle to begin with. There may be headache, light-headedness, dizziness, an increase in breathing rate and sweating. There can be a restriction in the field of vision, a sensation of numbness or tingling and feelings of euphoria.
Severe hypoxic/anoxic brain injury
As the degree of anoxia becomes more pronounced, confusion, agitation or drowsiness appear, along with cyanosis - a bluish tinge to the skin, reflecting the lowered oxygen content of the blood, often most apparent around the lips, mouth and fingertips. There may be brief jerks of the limbs (myoclonus) and seizures, both resulting from the damaging effects of lack of oxygen on the brain. If the anoxia is severe, it will result in loss of consciousness and coma.
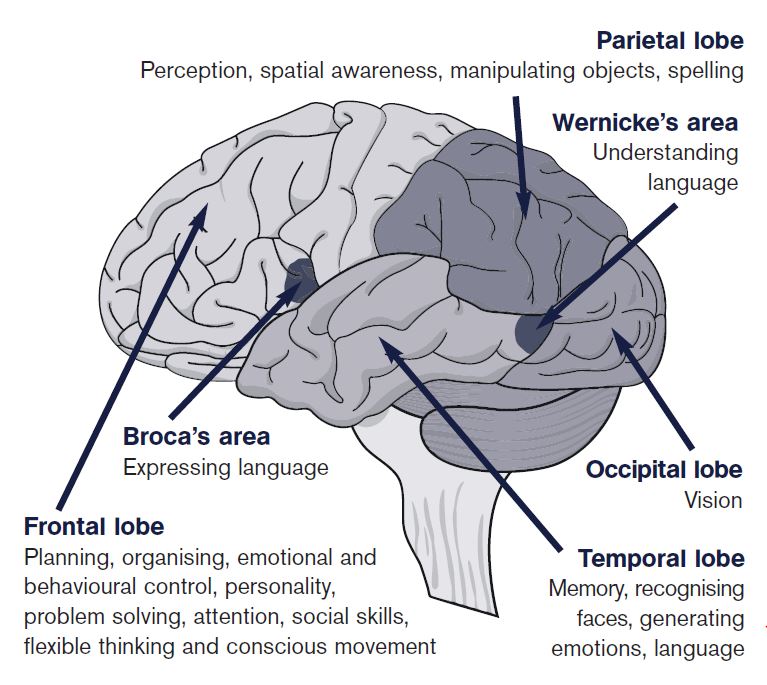
Because of their high demand for energy, the nerve cells of the brain are particularly sensitive to lack of oxygen. Although anoxia may produce damage to cells throughout the brain, some areas are more vulnerable than others. The cerebral cortex (especially the parietal lobes and occipital lobes), the hippocampus (important in memory), the basal ganglia and the cerebellum (both contributing to the control of movement) are particularly sensitive to anoxia.
When there is also an interruption of blood flow, as after a cardiac arrest, this may lead to damage in the areas furthest away from the territories supplied by the three major arteries of the brain. These 'watershed areas' are particularly vulnerable when blood flow is reduced and may suffer death of tissue (infarction), like that occurring in a stroke.
Severe anoxic brain injury may occasionally cause damage to the hypothalamus and pituitary gland, which are small structures at the base of the brain responsible for regulating the body's hormones. Damage to these areas can lead to insufficient or increased release of one or more hormones, which causes disruption of the body's ability to maintain a stable internal environment (homeostasis). In the early stages this can cause a condition called neurogenic diabetes insipidus, which is characterised by increased thirst and excessive production of dilute urine. This is due to a reduction in secretion of a hormone called vasopressin (anti-diuretic hormone) and can be treated by administering desmopressin (manufactured anti-diuretic hormone) and replacing lost fluids.
Cerebral anoxia may also produce brain swelling and this can add to the damage, by squeezing off smaller blood vessels and interrupting the local blood supply.
Reduced awareness states
If there has been very severe anoxic damage to the brain, there may be a transition from coma into a persistent vegetative state (PVS). In PVS the basic brain functions of breathing spontaneously, maintaining the heartbeat and blood pressure, digesting food and producing urine all continue. However, even though there may still be a cycle of sleeping and waking and the eyes may open spontaneously, there is no real evidence of consciousness in any meaningful sense and no response to what is going on in the environment.
More recently, the possibility of a minimally conscious state has been recognised. This is distinct from PVS, because although it is still a state of profoundly altered consciousness, there is minimal but definite evidence of some limited self-awareness or awareness of the surroundings.
Severe anoxic brain injury is often fatal. In cases where the injury is so severe that there is no chance of recovery doctors may put in place orders that the patient is not resuscitated in the event of further complications, such as cardiac arrest.
What are the long-term effects of hypoxic/anoxic brain injury?
The long-term consequences will depend on the severity of the cerebral anoxia and on how much irreversible damage has occurred in the brain. If there has only been mild or short-lived anoxia, there may well be recovery back to a normal or near normal level of functioning.
However, if the anoxic injury has been more marked the outcome is less certain and there are likely to be long-term effects. The nature of these problems will vary from person to person, depending on the severity of the injury and the brain areas affected.
There is considerable overlap with the effects of other kinds of acquired brain injury. However, the selective vulnerability of particular regions of the brain to anoxia also gives some distinctive features to this type of injury. A wide range of difficulties can occur, although not all are necessarily seen in every individual.
Physical effects
Damage to the cerebral cortex, the cerebellum and the basal ganglia may lead to limb weakness and disturbances of movement, balance and co-ordination. There may be spasticity or rigidity, with increased muscle tone. Anoxic injury to the basal ganglia may lead to abnormal movements, including tremor, involuntary writhing movements (athetosis) and brief, jerky movements (chorea).
Visual disorders
The occipital lobe at the back of the brain contains the main visual centres and it is particularly susceptible to anoxia, which may cause a loss of visual function referred to as cortical blindness. Damage to the occipital lobe may also lead to conditions such as Anton's syndrome. This is a rare condition, in which a patient with cortical blindness may show no awareness of the loss of vision and deny any problem, despite walking into things and showing obvious evidence of an inability to see normally. Conversely, patients may experience blindsight, in which they may respond to visual stimuli without being consciously aware of being able to see.
Memory problems
The hippocampus, on the inner surface of the temporal lobe, is an important structure for memory function and it is sensitive to anoxic injury. Memory problems are very common following cerebral anoxia and they may be quite severe.
Speech and language
Disturbances of speech and language function may occur because of damage to areas of the brain involved in the production and articulation of speech, finding the right words and understanding language. Spoken and written communication may both be affected.
Executive dysfunction
Damage to the frontal lobes may lead to disturbances in executive function - the ability to think and reason, to synthesize and integrate complex information and make considered judgements and decisions about what to do in a particular situation. These skills underlie the ability to plan for the future in a sensible way, as well as to function effectively in work and social settings.
Emotional and behavioural changes
Frontal lobe injury may produce changes in personality, including irritability, poor tolerance of frustration, impulsiveness and impairments in social perception and conduct. There may be apathy and lack of insight, as well as intermittent agitation and mood swings, or more sustained periods of depression. These changes may slow the progress of rehabilitation and make it difficult to achieve a successful return home.
Hormonal imbalances
Occasionally, severe anoxic injury can cause damage to the hypothalamus or pituitary gland, which can lead to a variety of hormonal problems, such as hypopituitarism. This is caused by a reduction in the release of hormones by the pituitary gland and symptoms include excessive tiredness, muscle weakness, decreased sex drive, inability to regulate body temperature, weight gain, low blood pressure, dry skin and headaches. Hormone replacement therapy can be used to treat hypopituitarism and other related disorders.
Get support from Headway
Headway offers a range of support to people with a brain injury, their family and friends. From a network of local groups and branches to specialist nurses, grants to individuals in need, a Brain Injury Identity Card and a nurse-led helpline.
Explore the Supporting you section to find out how we can help.
My story
Smart by name...
In January 2009, when she was just 16, Lizzie Smart was struck down by an infection in her throat, causing her brain to be starved of oxygen. But this determined young lady is not one to let anything stand in the way of her dreams.
Read storySupporting you
From local groups or branches, our Emergency Fund, Brain Injury Identity Card, helpline and much more, find out how Headway can support you after brain injury.
Find out more